Neurodevelopmental Disability
Among Children: Training Module of INDT-NMI Tool
Learning Objectives
- Overview of Neuromotor impairments
- Describe core symptoms of cerebral palsy, neuromuscular disorders and other neuromotor impairments
- Description of INDT-NMI tool
- Clinically evaluate a child with NMI using INDT-NMI tool
- Future research: Need for modified tool
What are Neuromotor Impairments (NMI)?
- NMI: Static or progressive difficulty in performing daily activities or coordinated movements
- Two pathology: UMN or LMN
- Three broad groups of NMI:
- Cerebral palsy
- Neuromuscular disease
- Other neuromotor impairment
Cerebral Palsy (CP)
- Disorder of tone, movement & posture
- Due to static or non-progressive disturbances that have occurred in the developing brain( e.g. birth asphyxia, kernicterus)
- Associated conditions
- Disturbances of sensation
- Disturbance of cognition
- Disturbance of communication
- Seizures
- Feeding problems
- Sleep disturbances
What is not Cerebral Palsy?
- Progressive neurological disorder
- Developmental regression
- Global developmental delay without any tone or movement abnormalities
- Transient tone and postural abnormalities which resolve by 1-2 years of age
- (e.g preterm children)
CP - Early Markers
Early Infancy
- Delayed attainment of milestones
- Excessive stiffness of limbs and/or trunk
- Abnormal twisting postures
- Persistence or a symmetry of Moro's & the ATNR beyond 6 months of age
- Early hand preference
- Cortical thumb
Later infancy & childhood
- Persistence of asymmetry in posture, movement &reflexes
- Excessive stiffness or abnormal twisting
- Persistent ATNR
- Delay in achieving milestones
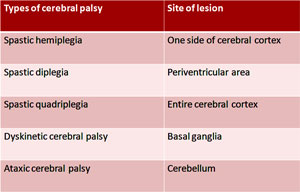
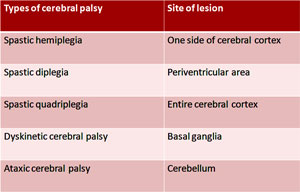
Topographical Classification
Co morbidity- Cerebral palsy
- Seizures
- Intellectual disability
- Feeding Difficulties
- Speech & Language Disorders
- Hearing Impairment
- Vision Impairment
- Inattention &/or Behavioural Problems
- Sleep Disturbances
Neuromuscular Disorders (NMD)
- Disorders resulting from pathology of the anterior horn cell, nerve roots, peripheral nerve, neuromuscular junction and/or the muscle
- These present with lower motor neuron (LMN) type of weakness
- Static or progressive or fluctuating course
- Manifest at different ages with a broad spectrum of symptoms, signs & variable severity
Common NMDs
- Muscular dystrophies
- Spinal muscular atrophy (SMA)
- Hereditary neuropathies
- Myasthenia gravis
- Acute flaccid paralysis (AFP)
- Paralytic poliomyelitis
- Guillain-Barre' syndrome (GBS)
- Transverse myelitis
- Traumatic neuritis
- Inflammatory myopathies
Neuromuscular Disorders
- Disorders of the
- Anterior horn cell (Neuronopathies)
- Peripheral nerve (Neuropathies)
- Neuromuscular junction (Myasthenia gravis)
- Muscle (Myopathies/Muscular dystrophies)
- Manifest at different ages with variable signs, symptoms and variable severity
- Hereditary or acquired
- Present with LMN type of weakness
Early Pointers to NMD
- Decreased fetal movement during antenatal period
- Floppy baby/infant
- Delay in attaining motor milestones
- Abnormal mode of walking (high stepping gait, toe walking or waddling gait)
- Difficulty in running, climbing stairs, getting up from the floor & frequent falls
- Enlargement/wasting of muscles
- Overt muscle weakness of recent origin
Other Neuromotor Impairments
- All conditions other than CP and NMD that cause weakness and/or problems in activity of daily living
- It includes:
- Sequelae of CNS infections
- Neural tube defects (NTDs) with sequelae
- Stroke and its sequelae
- Neurodegenerative disorders
- Acquired CNS demyelinating disorders
What is NOT Neuromotor Impairment?
- Developmental dysplasia of the hip
- Club foot (Congenital talipes equinovarus)
- Bone and joint disease: Trauma, infections of the joints (pyogenic or tubercular arthritis), rickets and rheumatoid arthritis
- Skin and soft tissue conditions: Painful lesions like in-growing toe nail, corn in the feet, ecthyma gangrenosum etc
- Contractures following burns or trauma
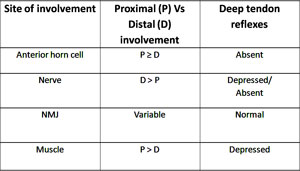
NMD & Other NMI: Clinical Spectrum
- Weakness:
- Weakness of limbs (usually legs)-abnormal gait, frequent falls and difficulty in performing ADL
- Delayed motor milestones
- Floppiness or stiffness of muscles
- Chronic proximal weakness
- Usually myopathies/muscular dystrophies (Except: Juvenile SMA)
- DTRs preserved but diminished
- Chronic distal weakness
- Usually neuropathies (Except: Myotonic muscular dystrophy)
- DTRs are absent
- Muscle fasciculations (esp. resting tongue)
- Associated sensory abnormality (sometimes
NMDs
Comorbidities: NMD & Other NMI
- Involvement of cardiac and respiratory muscles resulting in respiratory insufficiency and congestive cardiac failure
- Joint contractures
- Decubitus ulcers
- Spinal deformities
Burden of NMI (India)
- Prevalence estimate (INCLEN study)
- Rural: 1.60 (95% CI-1.10-2.31)
- Urban: 1.6 (95% CI-0.92-2.77)
- Every year 65,000 cases of cerebral palsy is being added to the existing population
- DMD is the most common Neuromuscular disorders in children
Need for early diagnosis and intervention
- Benefit from early diagnosis
- Early stimulation therapy
- Improved neurodevelopmental outcome
- Implication in prognosis especially in infants with NMI of genetic etiology (eg SMA/DMD)
Is Diagnostic tool Necessary?
- Lack of standardized Indian tool to diagnose NMI in India
- Correct diagnosis and prompt referral impact the outcome: Primary health care provider
- Early recognition by primary care provider: reduce the burden on tertiary care level
Principles of INDT-NMI Tool
- For any child presented with CNS complains thorough history taking and detailed CNS examination have pivotal role in diagnosis
- INDT-NMI tool is based on principles of focused history and CNS examination.
- A complete CNS examination is time taking and at times becomes a challenge in pediatric age group.
- Focused CNS examination tailored to child's complaint can obtain essential information for diagnosis while maintaining child's maximum cooperation.
Basic Neurological Examination Motor System Examination
Posture/Gait
- Normal
- Hypotonic
- Cross-legged
- Asymmetric i.e. hypertonic on one side (Hypertonia)
Muscle bulk/Nutrition
- Normal
- Atrophy
- Hypertrophy
Muscle power grading
- V: Normal power
- IV: Movement against some resistance
- III: Movement against gravity
- II: Movement eliminating gravity
- I: Flicker of movement Decreased muscle
- 0: No movement at all
Basic neurological Exam Motor System Examination
- Muscle tone
- Normal/Hypotonia/ Hypertonia (Spasticity or Rigidity)
- Distribution: Upper limb, lower limb,Trunk, Neck
- Deep tendon reflexes (biceps, triceps, supinator,
- knee and ankle jerks)
- Normal
- Diminished or absent
- Exaggerated
Basic Neurological Exam Motor System Examination-Reflex
- Corneal & Conjunctival reflex
- Abdominal reflex
- Cremasteric reflex
- Anal reflex
- Plantar response
- Flexor response/Not elicitable
- Extensor response
- Withdrawal of lower limb
Basic Neurological Exam
- Sensory system
- Touch
- Pain
- Temperature
- Vibration
- Proprioception
- Coordination
- Involuntary movements
- Meningeal signs
- Signs of raised ICT
- Cerebellar signs
- Ataxia
- Nystagmus
- Dysmetria
- Dysdiadochokinesia
- Tremors
- Spine and Skull examination
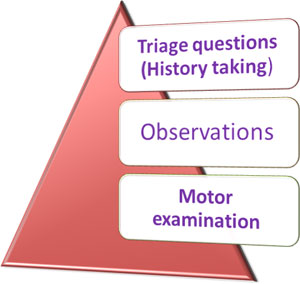
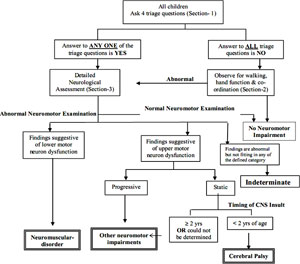
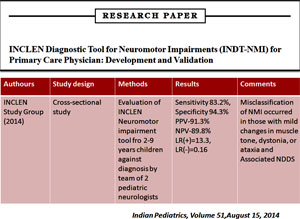
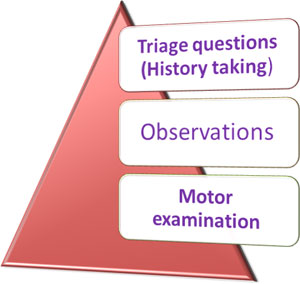
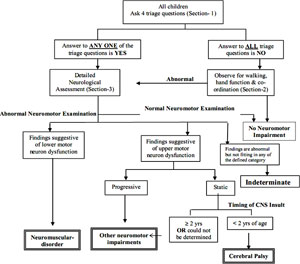
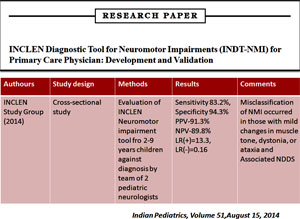
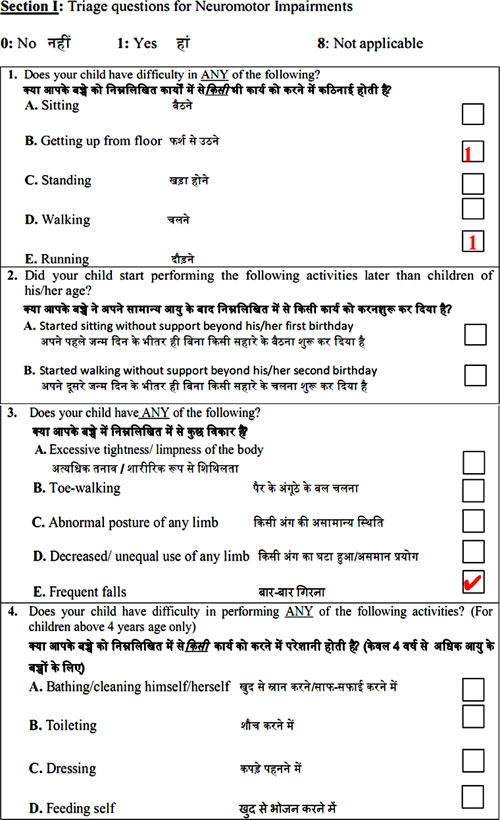
Overview of INDT-NMI Tool
- It consists of three sections:
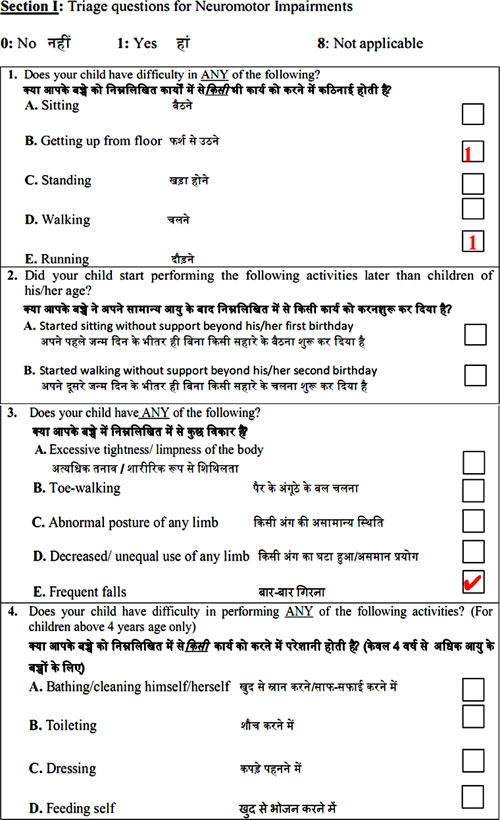
- Section-I (Triage questions) consists of four questions to elicit information from the parents/primary caregiver of the child regarding attainment of selected motor developmental milestones.
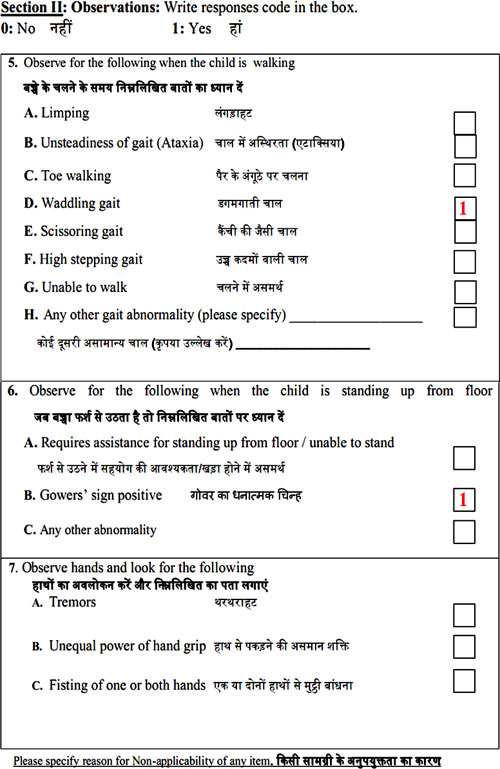
- Section-II (Observations): Physician makes three observations for assessing hand function, gait and muscle weakness.
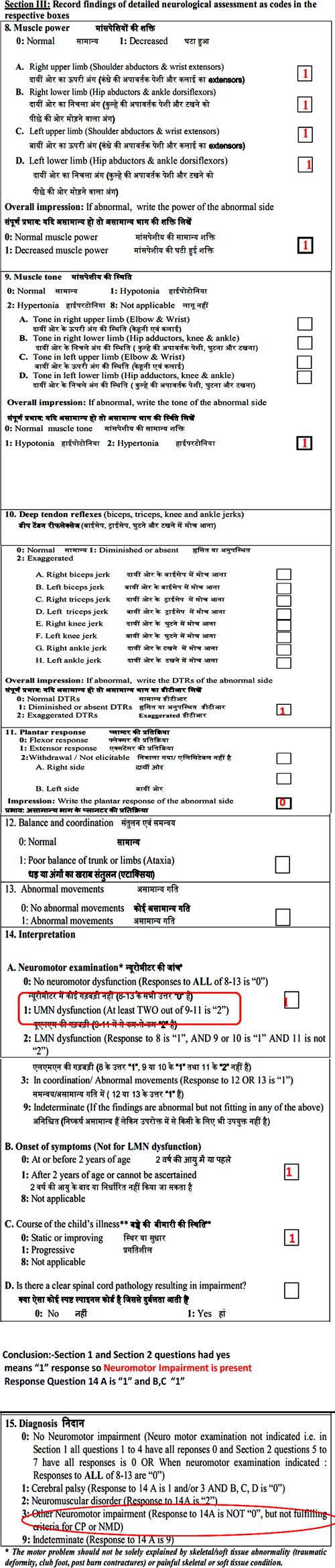
- Section-III consists of six questions, and the operator (graduate physician) does the neurological examination necessary for confirmation of NMI.
Overview of INDT-NMI Tool
- Thus final diagnosis of NMI is derived through an algorithm based on interpretation of three sections (i.e. 13 questions/items)
- The final diagnosis informs whether the case has:
- Cerebral palsy (CP)
- Neuromuscular disorders (NMD)
- Other NMI (that does not fit in to either CP or NMD)
- No NMI
- Indeterminate clinical condition
- This tool requires approximately 20-25 minutes for assessing each child
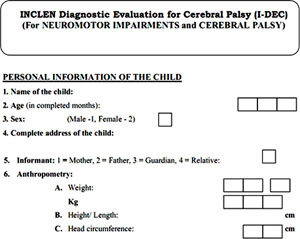
INDT-NMI Tool (Personal Information)
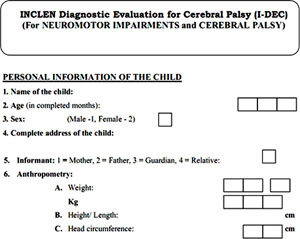
Tool Has 3 Parts
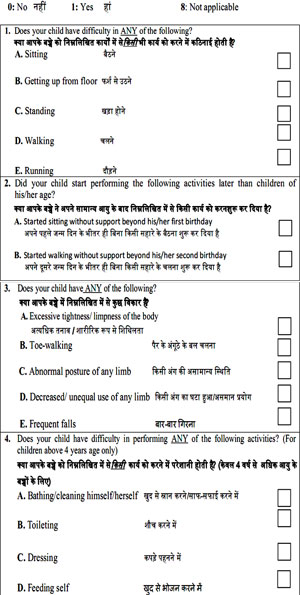
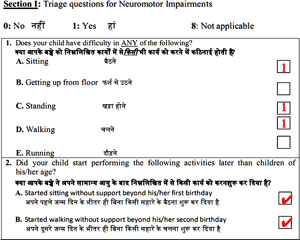
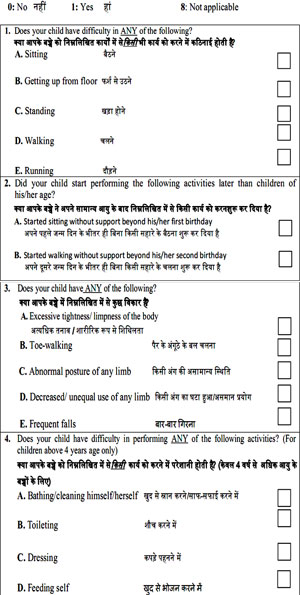
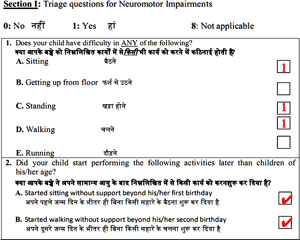
Triage Question: Question 1
- Does your child have difficulty in ANY of the following: Sitting/ getting up from sitting position/ Standing / Walking/ Running?
- How to ask: Ask each component of the question separately and wait for parent's response. After getting clear response, then move on to next component
- Mark YES: If the child has difficulty in ANY of the above listed activities or If the child has NOT ATTAINED that milestone
- Mark NO: If the child has no difficulty in the above activities
Triage Question: Question 2
- Did your child start performing the following activities later than children of his/her age (Sitting without support beyond his/her first birthday/ Walking without support beyond 2nd birthday)
- How to ask: Ask each component of the question separately and wait for parent's response. After getting clear response, then move on to next component.
- Mark YES: If the child had DELAY in attainment of these motor milestones
- If the child had NOT ATTAINED these milestones yet
- Mark NO: If the child had NO DELAY in attainment of these motor milestones
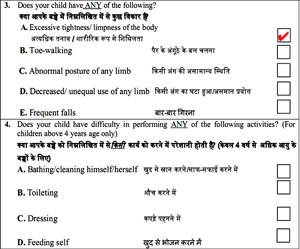
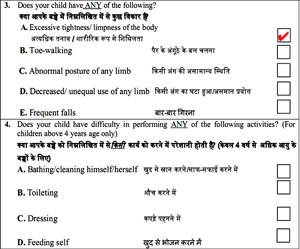
Triage Question: Question 3
- Does your child have ANY of the following?
- Excessive tightness or limpness of the body/ Toe-walking/ abnormal posture of any limb/ decreased or unequal use of any limb/ Frequent falls
- Mark YES: If the child has abnormality mentioned
- Mark NO: If the child has no abnormality as listed in the question
- Mark Not Applicable: for components “frequent falls” and toe walking” if the child is unable to walk or not yet attained walking
Triage Question: Question 4
- Does your child have difficulty in performing ANY of the following activities? (For children above 4 years age only)
- Bathing or cleaning self/ Toileting/ Dressing/ Feeding self
- How to ask: Ask each component of the question separately and wait for parent’s response. After getting clear response, then move on to next component.
- Mark YES: If there is difficulty in any of above listed activities
- NO: If the child has NO difficulty in any of the above activities
- Mark Not Applicable: For children between 2-4 years of age
- If parents say that “we have never allowed the child to do these tasks; we do this ourselves”
Triage questions for Neuromotor Impairments
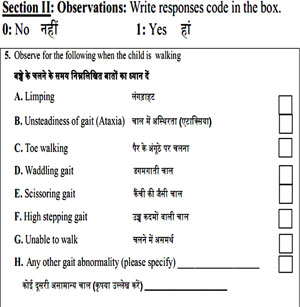
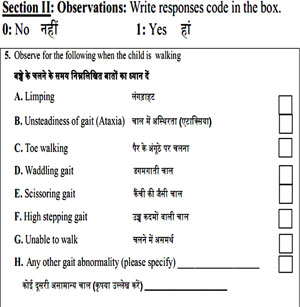
Observation based question: Question 5
- Observe for the following when the child is walking
- Limping
- Unsteadiness of gait (Ataxia)
- Toe walking
- Waddling gait
- Scissoring gait
- High stepping gait
- Unable to walk
Observation Based Question: Question 5
- How to test: Ask the child to walk across the room (at least 10 meters) comfortably and observe the gait. If you are attentive, you can also observe the gait when the child enters examination room.
- Mark as YES: If the child has any of the abnormal gait described above
- If the child is unable to walk
- Mark as NO: If the child's gait is normal
- Mark as Not Applicable: If the child has not attained walking yet
Hemiplegic Gait
Legend: Child is walking keeping her right upper limb adducted at shoulder, flexed at elbow and making circumduction arch with right lower limb which is suggestive of right sided hemiplegic gait
Spastic Couch Gait
Legend: Child is walking with his both lower limbs adducted at hips and flexed at knee suggestive of crouch gait observed in spastic diplegic CP
Neuropathic Gait
Legend: Observe the child walking by lifting the feet high from the floor. This gait is called high stepping seen in patients with peripheral neuropathy
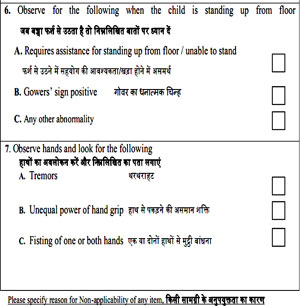
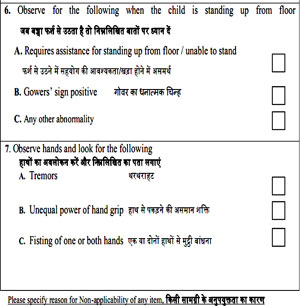
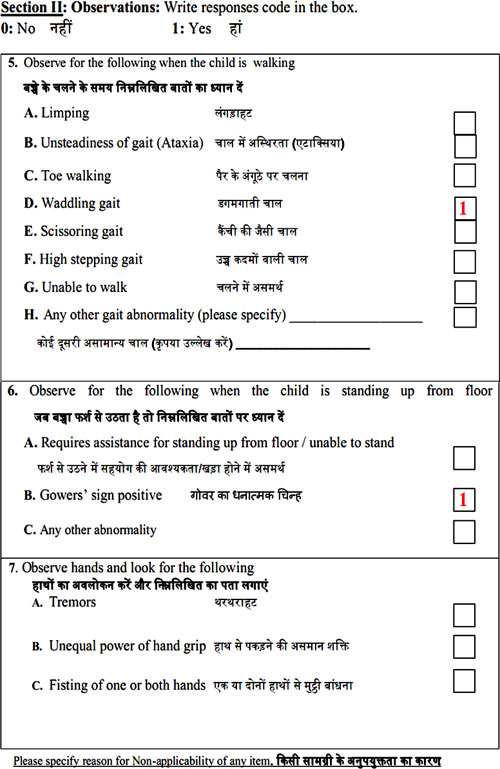
Observation Based Question: Question 6
- Observe for the following when the child is standing up from floor
- Requires assistance for standing up from floor or unable to stand/ Gowers' sign
Observation Based Question: Question 6
- How to test: Make the child sit down on the floor completely and then ask him/her to get up to standing position without holding the furniture.
- Mark as YES: If the child has difficulty in getting up from sitting on floor
- If the child requires assistance to stand from sitting position
- If the child has not learned standing yet
- If Gower's sign is positive
- Mark as NO: If the child has NO difficulty in getting up from sitting on floor
- If the child DOES NOT require assistance to stand from sitting
Observation Based Question: Question 6
Legend: On an attempt to raise up from the floor, child is observed to stand with support of his lower limb as if climbing on his on legs, this is called Gower sign
Observation Based Question: Question 7
- Observe hands and look for the following
- Tremors
- Unequal power of hand grip
- Fisting of one or both hands
- Tremors - Ask the child to stretch his/her arms and spread out the fingers
- Unequal power of hand grip - Ask the child to grasp your two fingers as forcefully as he/she can, while you try to separate your fingers
- Fisting of one or both hands - Observe during the course of examination
- Mark as YES: If the child has any of the above listed abnormalities in hands
- Mark as NO: If the child has none of the abnormalities in hands
When ASKED to STAND!!
Legend: observe the hand tremors in child having ITS(infantile tremor syndrome)
Legend: observe the twisting posture of hands suggestive of dystonia
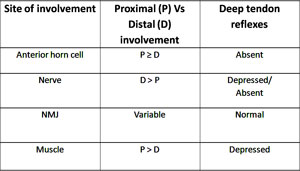
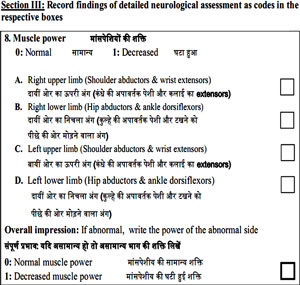
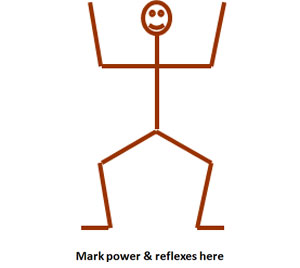
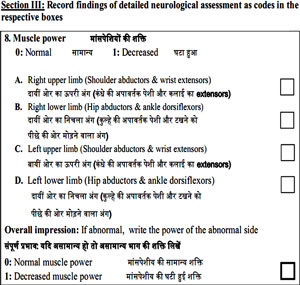
Motor examination: Question 8
- Muscle Power
- How to test: Test at least two muscles in each limb and note down the power whether normal or decreased. In upper limbs, shoulder abductors and wrist extensors are to be tested; and in lower limbs hip extensors and ankle dorsiflexors are to be tested.
Description of muscle power: question 8
- Description: Muscle power is the strength of the muscle. This is graded as follows:
- 5-Normal (movement against gravity and full resistance)
- 4-movement against gravity and some resistance
- 3-Movement against gravity but not against additional resistance
- 2-Movement with gravity eliminated
- 1-Visible or palpable flicker of contraction but no visible movement of the part/joint
- 0-No movement at all
- Any grade from 0-4 is recorded as decreased muscle power
Muscle group |
Testing position |
How to test |
Shoulder abductors |
Sitting |
Ask the child to elevate arms above the level of head; try to counter this by applying some pressure at elbow |
Wrist extensors |
Sitting with hand kept flat on table top |
Ask the child to lift the wrist up forcefully against your hand |
Hip extensors |
Prone position |
Ask the child to lift knee from couch and hold it up. Place your hand on popliteal fossa and try to press it down with slight resistance |
Ankle dorsiflexors |
Sitting with legs hanging from couch |
Ask the child to dorsiflex ankle against resistance by your hand placed over dorsum of foot |
Power Assessment - Sitting
Legend: Observe how to test neck flexors
Legend: Observe how to test shoulder abductors and adductors
Power Assessment - Sitting
Legend: Observe how to test elbow and wrist flexors and extensors
Legend: Observe how to test elbow extensors by eliminating gravity and shoulder abductors
Power Assessment - Sitting
Legend:: Observe how to test hip flexors
Legend: Observe how to test knee extensors
Power Assessment – Side Lying
Legend:: observe how to test Hip adductors and abductors in side lying position
Power Assessment - Prone
Legend:: Observe how to test neck extensor
Legend: Observe how to test knee flexor and ankle plantar flexors
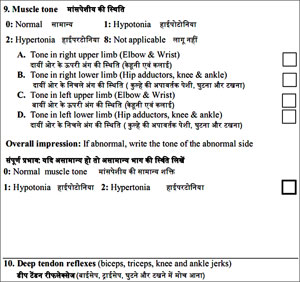
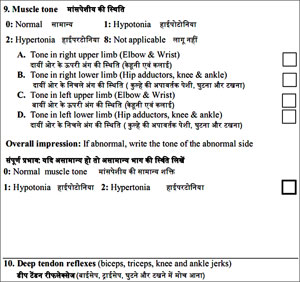
Motor examination: Question 9
- Muscle Tone
- 0: Normal
- 1: Hypotonia
- 2: Hypertonia
- How to test:
- See the posture of limbs: frog-like posture or scissoring
- Feel the muscle
- Do: Passive movements of the joints and range of motion at the joints.
- Interpretation:
- Flappability
- Spasticity:
- UL → pronation and supination; pronator catch
- LL→ hip extensors, knee extensors & plantar flexors of foot
Motor Examination: Question 9
Legend: Observe the assessment of tone by passive flexion across the joints
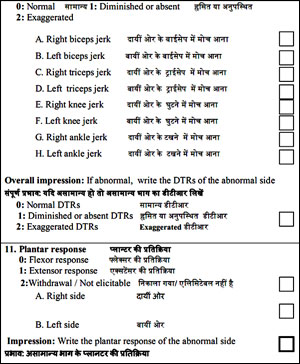
Motor examination: Question 10
- Deep tendon reflexes (biceps, triceps, knee and ankle jerks)
- 0: Normal
- 1: Diminished or absent
- 2: Exaggerated
- You should elicit DTRs at biceps and triceps in UL, and knee & ankle in LL.
- DTRs are grades as follows
- 0: absent
- 1+: Sluggish or reduced
- 2+: normal
- 3+: Exaggerated
- 4+: Brisk with presence of clonus
Motor Examination: Question 10
Legend:: : Observe how to elicit DTR
Legend: Observe the clonus
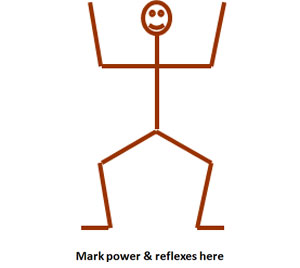
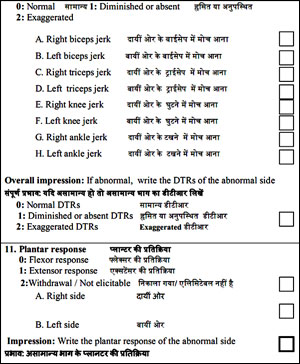
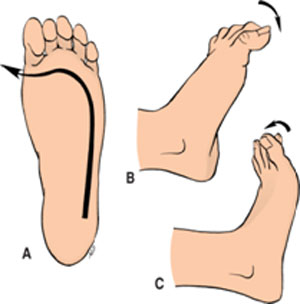
Motor Examination: Question 11
- Plantar Response
- How to test: Gently draw a blunt stimulus along the lateral border of the sole. Watch the big toe and remainder of the toes. Possible responses are as follows:
- Interpretation
- All toes flex - Flexor response
- Extension of great toe and fanning of other toes - Extensor plantar response
- No movement - Not elicitable
- Big toe extends, other toes extend, ankle dorsiflexion - Withdrawal response
Observe to Elicit the Plantar Response
Motor Examination: Question 12
- Balance and Coordination
- 0: Normal
- 1: Poor balance of trunk or limbs (Ataxia)
- How to test: Truncal ataxia is seen as swaying/unsteadiness while sitting
- Ataxic gait can be identified by asking the child to walk
Motor examination: Question 13
- Abnormal Movements
- 0: No abnormal movements
- 1: Abnormal movements
- Abnormal movements observed in children with dyskinetic cerebral palsy includes:
- Choreoathetoid movements
- Dystonia
- Tremor
- Ballismus
Motor System Examination
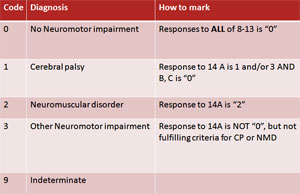
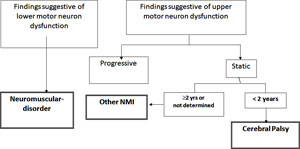
(Question 8-13) Interpretation
A: Neuromotor Impairment
- 0: No neuromotor dysfunction (Responses to ALL of 8-13 is “0”)
- 1: UMN dysfunction (At least TWO out of 9-11 is “2”)
- 2: LMN dysfunction (Response to 8 is “1”, AND
response to 9 or 10 is 1 AND 11 is not 2
- 3: In coordination/ Abnormal movements (Response to 12 OR 13 is “1”)
- 9: Indeterminate (If the findings are abnormal but not fitting in any of the above)
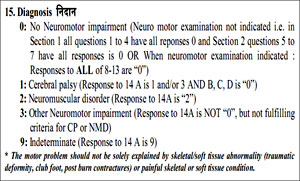
14: Interpretation
- B. Onset of symptoms (Only for UMN dysfunction)
- 0: At or before 2 years of age
- 1: After 2 years of age or cannot be ascertained
- 8: Not applicable
- C. Course of the child's illness
- 0: Static or improving
- 1: Progressive
- 8: Not applicable
- D. Is there a clear Spinal cord pathology resulting in impairment

Final Interpretation of INDT-NMI Tool
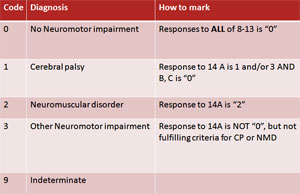
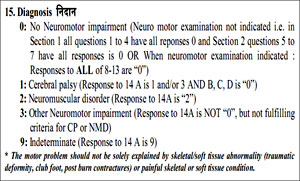
Consensus Clinical Criteria-Cerebral palsy
Cerebral palsy is characterized by ALL of the following:
- Predominant motor impairment with abnormalities of (one or more of the following)
- Non-progressive in nature
- Onset before two years of age
- Cerebral in origin
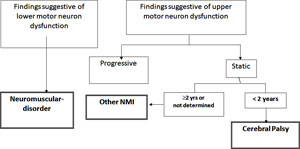
Consensus Clinical Criteria-NMD and Other NMI
Probable diagnosis of NMD / Other NMI is made only if both A and B are fulfilled |
A |
Static or progressive difficulty in performing activities of daily living or coordinated movements. |
B |
ANY of the following is present-
- Findings suggestive of static or progressive LMN dysfunction (NMD)
- Findings suggestive of progressive UMN dysfunction (Other NMI)
- Static UMN dysfunction with onset after age of two years (Other NMI)
|
Interpretation of Examination Findings
Additional Information
- Probable timing of insult
- < 2 years
- ≥ 2 years age or can not be ascertained
- Course of the illness
- Static or improving
- Progressive
- Intelligence
- Apparently normal
- Mental retardation
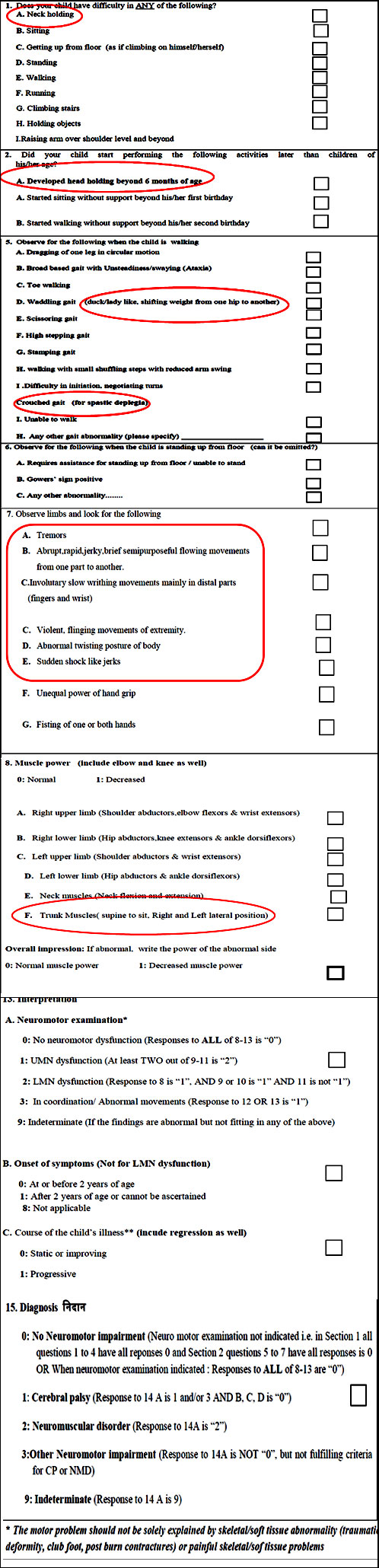
Case Vignette
A 3 year old boy presented with
- Delay in attaining developmental milestones.
- He attained neck holding at the age of 10 months
- Sitting without support at 18 months
- Walking unassisted at 2 ½ years of age
- He can not feed by himself properly and spills the food.
- He has age appropriate social-adaptive development
- Speaks 2 word sentences like “give water”
- He was born to a primigravida mother at 33 weeks gestation and developed severe jaundice on day 4 of life, requiring phototherapy for about 72 hour but never had seizures
- There were no similar problems in the family members


Case Vignette
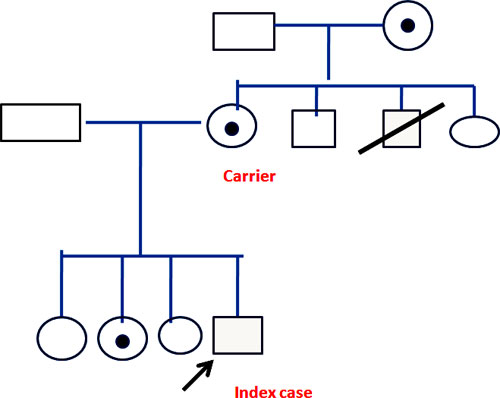
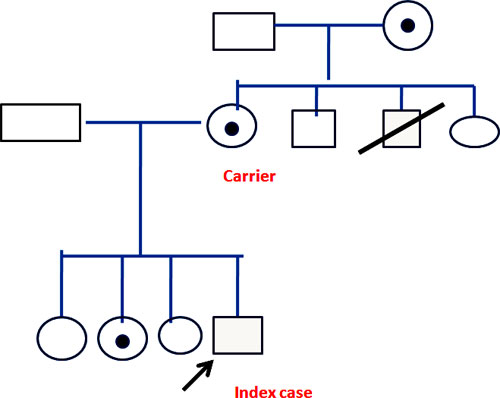
- A 8 year old boy
- Presented with difficulty in walking
- He was apparently normal till 6 years of age and started going to school also.
- His difficulty in walking is gradually worsening and at present, he is unable to walk without assistance
- He has difficulty in walking upstairs and standing from sitting position
- Other than this, he has no other problems. He is average in studies.
- One of mother's two brothers (child's maternal uncle) had similar problem at the age of 7 years and he died at 14 years of age
Pedigree Chart
Gower's Sign
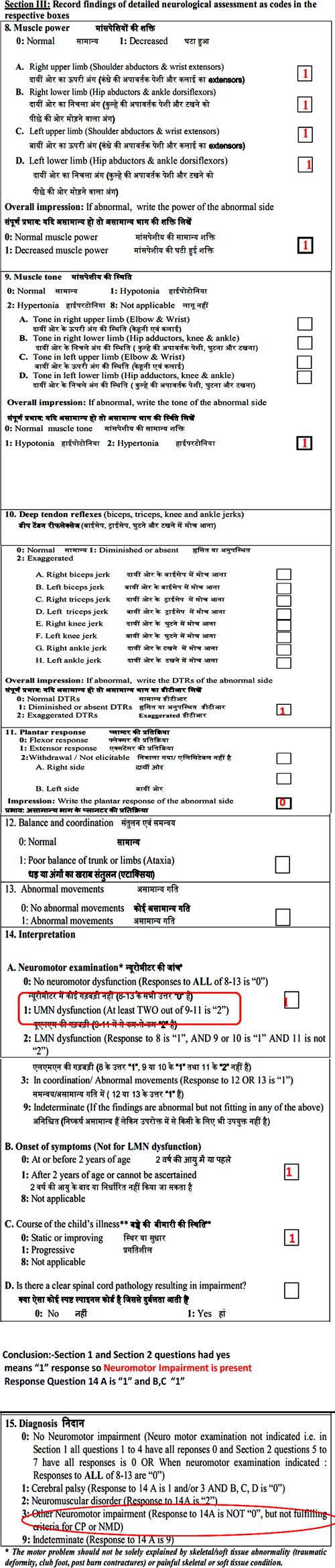
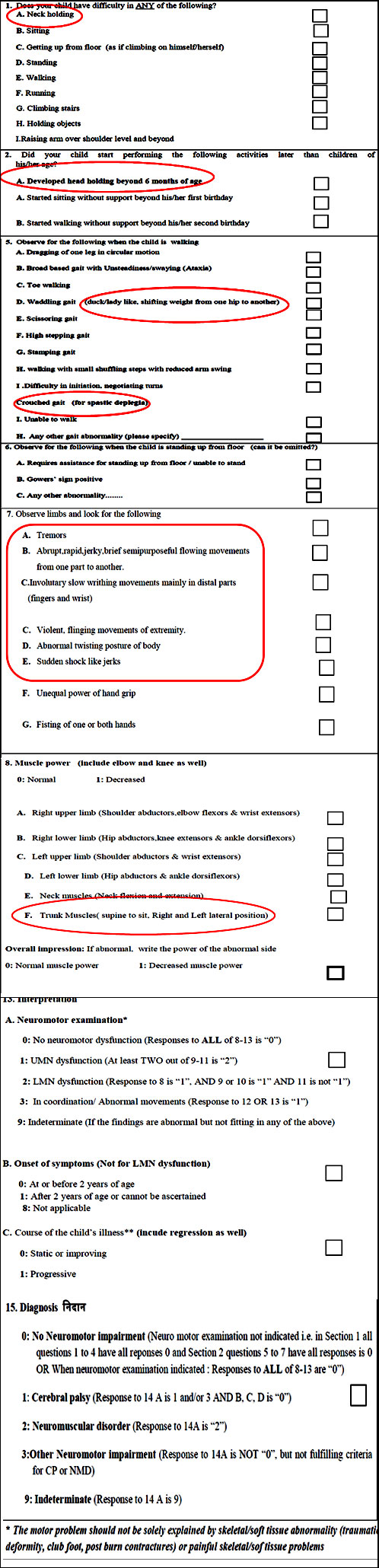
Modified INDT- NMI Tool
- Why modified?
- Age group broaden to 0-18 years children
- Detailed description of symptoms and signs of cerebellum and extrapyramidal involvement
What Would Change In INDT-NMI Tool
Summary
- Neuromotor impairment has three broad groups: cerebral palsy, neuromotor disease, other NMI
- Need for early diagnosis and early referral
- INDT-NMI is useful tool for diagnosis of NMI by primary care physician
- Need for modified tool based on broader age group